Sleep is not merely a period of rest; it is a complex physiological process influenced by various factors, including the vibrant ecosystem within our gut: the microbiome. This article explores the fascinating world of gut bacteria and their surprising impact on our sleep patterns.
INTRODUCTION TO SLEEP
Sleep is essential for hormonal regulation, particularly for melatonin and cortisol, which govern our sleep-wake cycles. Melatonin, the “sleep hormone,” is produced by the pineal gland and signals the body to prepare for sleep. As night falls, melatonin levels rise, inducing drowsiness and lowering body temperature to facilitate sleep (1, 2). Cortisol, the “stress hormone,” is secreted by the adrenal glands and promotes morning alertness. Its levels peak at dawn and decrease by evening, aiding the transition to sleep (3). This hormonal interplay is crucial to our circadian rhythm, the internal clock that orchestrates our physiological processes over a 24-hour cycle, essential for healthy sleep patterns (4, 5).
Disrupted sleep can disturb this hormonal balance, impairing overall health. Insufficient or poor-quality sleep can increase nighttime cortisol (6), disrupting sleep and perpetuating stress and insomnia. This hormonal imbalance can also affect hunger-related hormones like ghrelin and leptin (7), potentially leading to overeating and weight gain. Prolonged sleep disturbances may even impact growth, thyroid, and reproductive hormones (8-9), with significant health consequences. The clinical importance of stable sleep patterns is underscored by the numerous health issues associated with sleep disruption, including cardiometabolic diseases (10-11), weight gain, metabolic syndrome, cancer (6,12-13), gastrointestinal problems, cognitive impairments (14-17), and reproductive health concerns (18-21).
Insomnia: The Silent Hormonal Disruptor
Insomnia, a common sleep disorder, is characterized by difficulty falling asleep, staying asleep, or both, and can profoundly affect hormonal balance. It can lead to an increase in stress hormones like cortisol, which may cause a cascade of stress-related issues and metabolic syndrome (22). The lack of restorative sleep associated with insomnia can decrease the secretion of growth hormone, essential for growth, metabolism, and muscle repair (8). Addressing sleep disorders such as Obstructive Sleep Apnea (OSA) and insomnia is crucial for maintaining hormonal health and overall well-being.
Sleep Apnea: A Disruptor of Hormonal Balance
OSA is a particularly disruptive sleep disorder that can exacerbate hormonal imbalances. OSA is characterized by repeated episodes of reduced airflow or pauses in breathing during sleep, leading to fragmented sleep and reduced oxygen levels in the blood (23). This can trigger a stress response, resulting in increased levels of stress hormones (24). Additionally, OSA is associated with a higher risk of developing metabolic and endocrine disorders such as hypogonadism, hypercortisolism, and osteoporosis, which can further complicate the hormonal landscape (25). The impact of OSA on hormonal balance highlights the importance of diagnosing and treating this sleep disorder to maintain hormonal health and overall well-being.
THE GUT MICROBIOTA-GUT-BRAIN AXIS
The gut microbiome influences sleep through its effects on immune biomarkers, neurotransmitter and hormone production, and metabolic alterations, highlighting the potential of modulating the gut microbiome to enhance sleep quality. The microbiome is vital for neurotransmitter synthesis, the chemical messengers crucial for mood, anxiety, and sleep regulation. Here’s an overview of this intricate process:
Microbial Metabolites: Certain gut bacteria, like specific Lactobacilli and Bacteroides strains, produce gamma-aminobutyric acid (GABA), a neurotransmitter known for its stress-reducing and sleep-promoting properties (26-27).
Precursor Synthesis: The microbiota can also affect neuro-active metabolite production by synthesizing precursors, such as tryptophan, which leads to serotonin production. Serotonin, a neurotransmitter associated with wakefulness, is converted to melatonin in the evening, initiating sleep (28-29).
Blood-Brain Barrier Penetration: Metabolites like short-chain fatty acids (SCFAs) from gut bacteria can cross the blood-brain barrier, potentially contributing to central nervous system neurotransmitter biosynthesis (30-31).
Immune System Modulation: Bacteria-derived signals can modulate immune responses, including cytokine production. Cytokines, capable of crossing the blood-brain barrier, can affect sleep regulation and circadian rhythms, indicating bidirectional communication between the immune system and sleep (32-33).
The Gut-Brain Axis bidirectional communication system allows gut microbiota to impact brain function and behavior, including neurotransmitter regulation, influencing sleep patterns and quality (34-35).
THE GUT MICROBIOME AND SLEEP: A SCIENTIFIC PERSPECTIVE
Exploring the Link Between Gut Health and Sleep
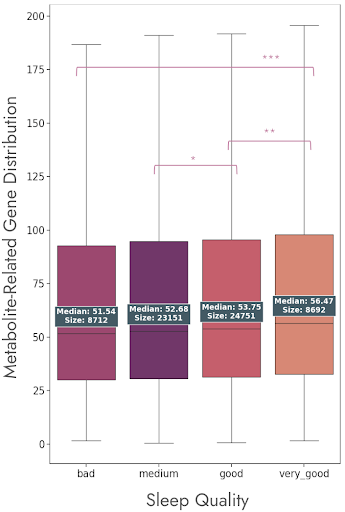
Digging into data from DayTwo’s extensive database of 90,000(!) users with sequenced microbiome data, we revealed notable links between microbial genes for metabolite production and the quality of sleep reported by participants. These individuals rated their sleep experience on a spectrum ranging from ‘bad’ to ‘very good.’ Such subjective assessments were then meticulously examined to identify microbial patterns associated with better or poorer sleep quality.
Looking at the genes of these microbes, we find that some are more abundant in people who sleep well, while others are more common in those who don’t. A statistical test showed that these differences are not just by chance – they’re significant. This means that there’s a real connection between the microbes in our gut and how we sleep.
Gut Bacteria Imbalance and Sleep Disruption
It’s becoming increasingly clear that the balance of bacteria in our gut is closely linked to sleep disorders like insomnia and sleep apnea. Research diving into DayTwo’s database, which includes the full medical records of around 30,000 people, has shed light on this fascinating link.
People with sleep disorders like insomnia and sleep apnea have a different mix of gut bacteria compared to those who sleep soundly. The diagrams below compare the levels of specific bacteria in those with sleep disorders to those without. The trend is clear: lower levels of certain bacteria are common in those who have trouble sleeping.
This isn’t just a random finding. The data shows a significant difference, pointing to gut bacteria imbalance as a possible player in sleep problems. It’s a reminder that our bodies are interconnected systems, and what happens in our gut can have far-reaching effects, even on our sleep.
ENHANCING SLEEP QUALITY BY IMPROVING THE MICROBIOME
Personalized medicine suggests that gut-based treatments could be customized to address individual sleep issues. By understanding our gut microbiota’s unique composition, we can implement lifestyle adjustments to promote a sleep-friendly environment. Regular sleep schedules, stress reduction, and a calming bedtime routine can balance cortisol levels and foster a healthy sleep-wake cycle. Practices like screen time moderation, meditation, aromatherapy, and sleep hygiene can positively impact the gut microbiome and sleep. Nutritionally, consuming fermented foods or those rich in prebiotic fibers can encourage the growth of beneficial gut bacteria (35-36).
The nexus between the gut microbiome and sleep is a burgeoning research field, offering novel strategies for sleep quality enhancement. By tailoring our lifestyle and dietary habits, we can harness this connection for better sleep and overall well-being.
REFERENCES
- Cajochen, C., Kräuchi, K., & Wirz‐Justice, A. (2003). Role of melatonin in the regulation of human circadian rhythms and sleep. Journal of neuroendocrinology, 15(4), 432-437.
- Cipolla-Neto, J., & Amaral, F. G. D. (2018). Melatonin as a hormone: new physiological and clinical insights. Endocrine reviews, 39(6), 990-1028.
- O’Byrne, N. A., Yuen, F., Butt, W. Z., & Liu, P. Y. (2021). Sleep and circadian regulation of cortisol: a short review. Current opinion in endocrine and metabolic research, 18, 178-186.
- Moon, E., Kim, K., Partonen, T., & Linnaranta, O. (2022). Role of melatonin in the management of sleep and circadian disorders in the context of psychiatric illness. Current Psychiatry Reports, 24(11), 623-634.
- Zisapel, N. (2018). New perspectives on the role of melatonin in human sleep, circadian rhythms and their regulation. British journal of pharmacology, 175(16), 3190-3199.
- Dickerson, S. S., Connors, L. M., Fayad, A., & Dean, G. E. (2014). Sleep–wake disturbances in cancer patients: narrative review of literature focusing on improving quality of life outcomes. Nature and science of sleep, 85-100.
- Otte, J. L., Carpenter, J. S., Manchanda, S., Rand, K. L., Skaar, T. C., Weaver, M., … & Landis, C. (2015). Systematic review of sleep disorders in cancer patients: can the prevalence of sleep disorders be ascertained?. Cancer medicine, 4(2), 183-200.
- Beroukhim, G., Esencan, E., & Seifer, D. B. (2022). Impact of sleep patterns upon female neuroendocrinology and reproductive outcomes: a comprehensive review. Reproductive Biology and Endocrinology, 20(1), 16.
- Goldstein, C. A., & Smith, Y. R. (2016). Sleep, circadian rhythms, and fertility. Current Sleep Medicine Reports, 2, 206-217.
- Qasrawi, S. O., & BaHammam, A. S. (2024). Role of Sleep and Sleep Disorders in Cardiometabolic Risk: a Review and Update. Current Sleep Medicine Reports, 1-17.
- Zhang, C., & Qin, G. (2023). Irregular sleep and cardiometabolic risk: Clinical evidence and mechanisms. Frontiers in Cardiovascular Medicine, 10, 1059257.
- Al Maqbali, M., Al Sinani, M., Alsayed, A., & Gleason, A. M. (2022). Prevalence of sleep disturbance in patients with cancer: a systematic review and meta-analysis. Clinical nursing research, 31(6), 1107-1123.
- Büttner-Teleagă, A., Kim, Y. T., Osel, T., & Richter, K. (2021). Sleep disorders in cancer—a systematic review. International journal of environmental research and public health, 18(21), 11696.
- Kong, J., Zhou, L., Li, X., & Ren, Q. (2023). Sleep disorders affect cognitive function in adults: an overview of systematic reviews and meta-analyses. Sleep and Biological Rhythms, 21(2), 133-142.
- Xu, W., Tan, C. C., Zou, J. J., Cao, X. P., & Tan, L. (2020). Sleep problems and risk of all-cause cognitive decline or dementia: an updated systematic review and meta-analysis. Journal of Neurology, Neurosurgery & Psychiatry, 91(3), 236-244.
- Casagrande, M., Forte, G., Favieri, F., & Corbo, I. (2022). Sleep quality and aging: A systematic review on healthy older people, mild cognitive impairment and Alzheimer’s disease. International journal of environmental research and public health, 19(14), 8457.
- Pearson, O., Uglik-Marucha, N., Miskowiak, K. W., Cairney, S. A., Rosenzweig, I., Young, A. H., & Stokes, P. R. (2023). The relationship between sleep disturbance and cognitive impairment in mood disorders: A systematic review. Journal of affective disorders, 327, 207-216.
- Zhao, J., Chen, Q., & Xue, X. (2023). Relationship between sleep disorders and female infertility among US reproductive-aged women. Sleep and Breathing, 27(5), 1875-1882.
- Potter, G. D., Skene, D. J., Arendt, J., Cade, J. E., Grant, P. J., & Hardie, L. J. (2016). Circadian rhythm and sleep disruption: causes, metabolic consequences, and countermeasures. Endocrine reviews, 37(6), 584-608.
- Rogers, E. M., Banks, N. F., & Jenkins, N. D. (2024). The effects of sleep disruption on metabolism, hunger, and satiety, and the influence of psychosocial stress and exercise: A narrative review. Diabetes/metabolism research and reviews, 40(2), e3667.
- Dorsey, A., De Lecea, L., & Jennings, K. J. (2021). Neurobiological and hormonal mechanisms regulating women’s sleep. Frontiers in neuroscience, 14, 625397.
- Andersen, M. L., Hachul, H., Ishikura, I. A., & Tufik, S. (2023). Sleep in women: a narrative review of hormonal influences, sex differences and health implications. Frontiers in Sleep, 2, 1271827.
- Maniaci, A., La Via, L., Pecorino, B., Chiofalo, B., Scibilia, G., Lavalle, S., & Scollo, P. (2024). Obstructive Sleep Apnea in Pregnancy: A Comprehensive Review of Maternal and Fetal Implications. Neurology International, 16(3), 522-532.
- Gottlieb, D. J., & Punjabi, N. M. (2020). Diagnosis and management of obstructive sleep apnea: a review. Jama, 323(14), 1389-1400.
- Saaresranta, T., & Polo, O. (2003). Sleep-disordered breathing and hormones. European Respiratory Journal, 22(1), 161-172.
- Tette, F. M., Kwofie, S. K., & Wilson, M. D. (2022). Therapeutic anti-depressant potential of microbial GABA produced by Lactobacillus rhamnosus strains for GABAergic signaling restoration and inhibition of addiction-induced HPA axis hyperactivity. Current Issues in Molecular Biology, 44(4), 1434-1451.
- Kaur, S., Sharma, P., Mayer, M. J., Neuert, S., Narbad, A., & Kaur, S. (2023). Beneficial effects of GABA-producing potential probiotic Limosilactobacillus fermentum L18 of human origin on intestinal permeability and human gut microbiota. Microbial Cell Factories, 22(1), 256.
- Potter, K., Gayle, E. J., & Deb, S. (2023). Effect of gut microbiome on serotonin metabolism: a personalized treatment approach. Naunyn-Schmiedeberg’s Archives of Pharmacology, 1-14.
- Kaur, H., Bose, C., & Mande, S. S. (2019). Tryptophan metabolism by gut microbiome and gut-brain-axis: an in silico analysis. Front Neurosci 13: 1365.
- Silva, Y. P., Bernardi, A., & Frozza, R. L. (2020). The role of short-chain fatty acids from gut microbiota in gut-brain communication. Frontiers in endocrinology, 11, 508738.
- Sahu, N., Upadhyay, P., & Mishra, S. K. (2022). Role of Short-Chain Fatty Acids from Gut Microbiota in Neuroendocrine Pathogenesis Management. In Gut Microbiome in Neurological Health and Disorders (pp. 139-151). Singapore: Springer Nature Singapore.
- Liu, Y., Wang, J., & Wu, C. (2022). Modulation of gut microbiota and immune system by probiotics, pre-biotics, and post-biotics. Frontiers in nutrition, 8, 634897.
- Sittipo, P., Choi, J., Lee, S., & Lee, Y. K. (2022). The function of gut microbiota in immune-related neurological disorders: A review. Journal of Neuroinflammation, 19(1), 154.
- Dos Santos, A., & Galiè, S. (2024). The Microbiota–Gut–Brain Axis in Metabolic Syndrome and Sleep Disorders: A Systematic Review. Nutrients, 16(3), 390.
- Smith, R. P., Easson, C., Lyle, S. M., Kapoor, R., Donnelly, C. P., Davidson, E. J., … & Tartar, J. L. (2019). Gut microbiome diversity is associated with sleep physiology in humans. PloS one, 14(10), e0222394.
- Haarhuis, J. E., Kardinaal, A., & Kortman, G. A. M. (2022). Probiotics, prebiotics and postbiotics for better sleep quality: A narrative review. Beneficial Microbes, 13(3), 169-182.